Medical Equipment Program
Reliable medical equipment is critical to delivering life-saving care.

Reliable medical equipment is critical to delivering life-saving care.
Safeguarding the availability, quality, and functionality of biomedical equipment in under-resourced health facilities.
The global development community invests billions of dollars in the deployment of medical equipment. However, without accounting for the many factors that can determine whether the equipment will achieve its intended impact, these investments often end up unused. Another WHO study found that over 50% of the medical equipment in low- and middle-income countries is either not functioning, not used correctly, or not maintained, with some being completely inadequate or unnecessary for its intended purpose.
As the global community bands together in response to COVID-19, medical equipment floods into under-resourced countries bringing an urgent need to ensure these investments results in sustainable returns—both in terms of health impacts and equipment performance. Without addressing these issues, even the best-intentioned solutions can be a burden to healthcare providers and end up in equipment graveyards around the world.
For over a decade, we have monitored and protected the vaccine cold chain using our award-winning sensor-based technologies. How can these same technologies safeguard other aspects of life-saving solutions, namely, biomedical equipment functionality, and both the availability and quality of power in health facilities?
With funding from the Bill and Melinda Gates Foundation and in partnership with Boston University and the Lata Medical Research Foundation, Nexleaf expanded the scope of our work to answer that question. We began by monitoring essential equipment, such as radiant warmers, phototherapy lights, oxygen concentrators, and other critical life-saving tools, used in neonatal intensive care units in three government hospitals in India. Continuously monitoring the utilization of medical equipment enabled us to uncover important insights about health care delivery that were previously unknown. For example, our sensor data showed that some equipment, such as baby radiant warmers, was turned off overnight. By speaking with the nurses, we learned ad hoc practices were employed due to mistrust of equipment.
This work was an eye-opening experience for our team and made one thing very clear: more needs to be done to understand how medical equipment can better serve the needs of health care providers in LMICs.

We are engaging global stakeholders, including equipment designers, manufacturers, distributors, maintenance providers, Ministries of Health, and critical care nurses, to better understand the gaps and challenges health care workers face. From these conversations, we have learned that there are needs around power quality, supply chains, human resources, training, and procurement that are not currently being met.
To date, equipment procurement funded by multinationals for lower-resource settings has primarily focused on the physical availability of the equipment, i.e., has the equipment reached a hospital setting. The industry standard is to claim impact after the equipment is procured, deployed, and installed. However, we know that real health impacts rely on more than a successful installation. Instead, it depends on considering the entire ecosystem that must be in place to ensure optimal efficiency and long-term equipment performance. Competency of health workers, availability of parts and consumables, and reliability of grid power or alternative power are all important factors.
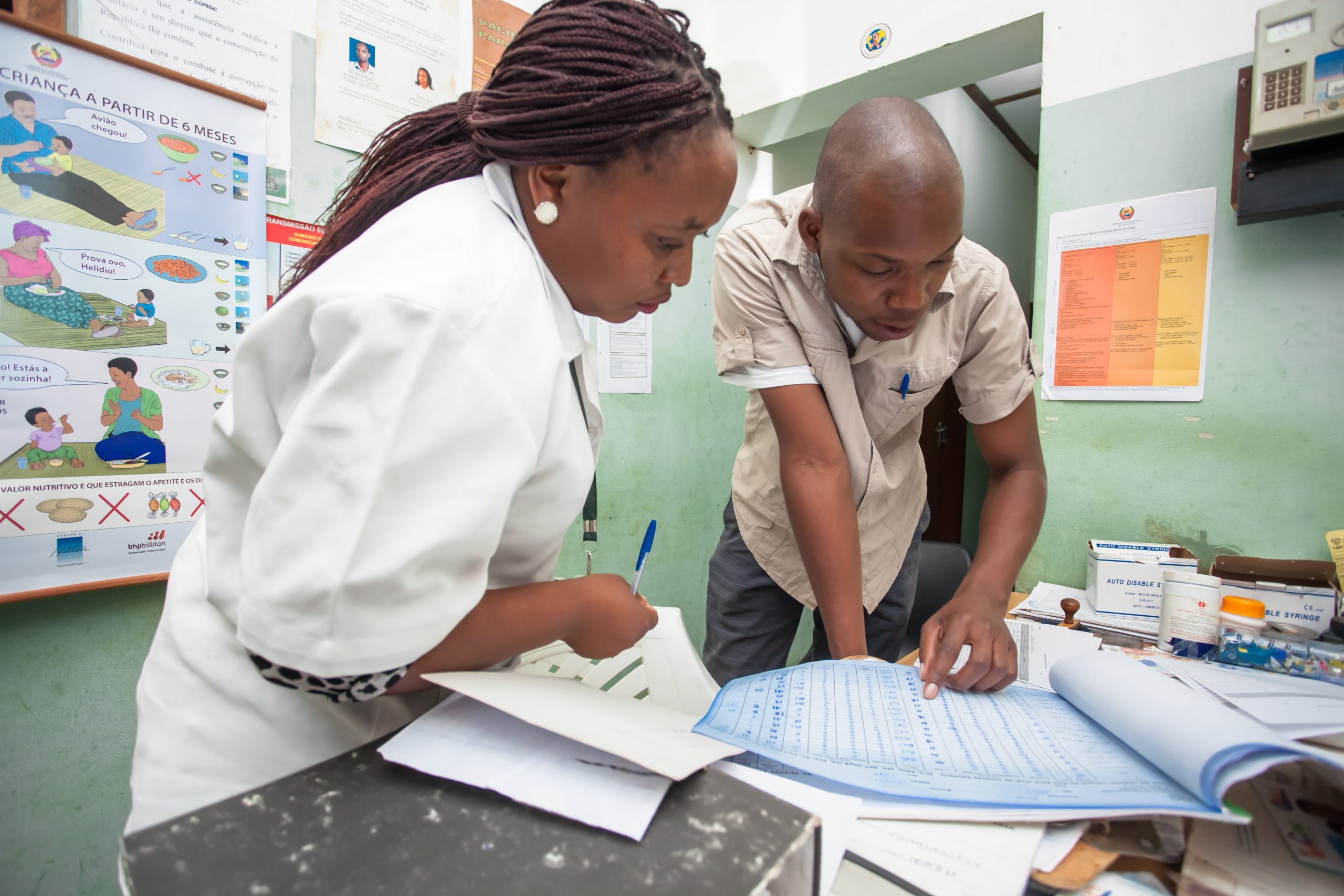
 Photo: World Bank / Vincent Tremeau
Photo: World Bank / Vincent Tremeau Health facilities around the world are faced with challenges that limit their ability to deliver safe and reliable care to their patients. Tackling issues like malfunctioning equipment, unreliable power availability, and overburdened staff is urgent in order to eliminate the health disparities that affect the poor. We help governments around the world build a digital framework using technology solutions and data analytics that supports traditional infrastructure and strengthens health systems.
The goal of this qualitative study was to understand challenges to SNCU care. In this paper, we focus on current gaps and future needs for SNCU equipment, quality of the power supply, and use of SNCU equipment.

Governments, foundations, and social enterprises that want to ramp up the production and distribution of medical equipment in response to COVID-19 and other ongoing threats need to assess the process holistically or risk overpromising and underdelivering on important aid for low- and middle-income countries.

Our partners at PagerDuty featured our collaborative work to support time-critical alerts in health facilities in Kenya in their first social impact report.

If you’re interested in learning more about our work or partnering with us, please contact Ednah Kiome at ednah@nexleaf.org.